Happy Tuesday, health heroes.
Last week we touched on the topic of inflammation. It’s a common malady, and sometimes, you may not even know you have it, let alone know what to do about it. That’s what this post today is for!
Let’s examine what inflammation might be trying to tell you and then consider what we can do about it.
You can catch up on the foundations of inflammation in my last post here:
To determine if you may have inflammation, ask yourself:
Do I often feel tired, brain-foggy, or sluggish?
Do I experience body aches or joint pain without explanation?
Are my digestive patterns irregular?
Do I have skin flare-ups, like eczema or rashes?
Do I get frequent infections?
Consider checking inflammatory markers, such as CRP, with your healthcare provider.
If the answer to any of these is yes, chronic inflammation might be a culprit.
Some less-obvious symptoms of inflammation might be easily dismissed or written off, like chronic fatigue, hair loss, gas and bloating, low-grade fever, heavy circles under your eyes (a sign of fluid retention and poor circulation), and even poor sleep quality.
Many of these symptoms are nebulous and hard to pinpoint, so if you experience them, continue to make mental notes. You know your body best, and recognizing symptoms like this can be helpful when being your own health detective.
Chronic inflammation, a persistent low-grade inflammatory response, can stem from numerous factors, making it a challenging puzzle to solve. On one side, vague symptoms often lack clear, measurable signs to help pinpoint the root cause. On the other, the multitude of potential triggers makes it difficult to determine which, if any, are truly responsible.
This can feel like trying to navigate without a clear sign pointing the way. In the case of inflammation, several paths could lead to potential causes, such as:
Poor diets that are high in sugar, trans fats, refined carbohydrates, and processed foods.
Physical inactivity and a sedentary lifestyle.
Chronic stress, whether emotional or physical, can dysregulate the immune system.
Sleep deprivation or low-quality sleep disrupts the body's natural repair processes.
Exposure to toxins, like chemicals, molds, and heavy metals.
Smoking and alcohol consumption, which we know, leads to inflammation in the liver and other organs.
Bacterial, viral, or fungal infections that are not fully eradicated can result in prolonged inflammation.
Gut dysbiosis. An imbalance in gut microbiota can trigger inflammation in the gastrointestinal tract and beyond.
Autoimmune disorders, like rheumatoid arthritis, lupus, and multiple sclerosis, involve the immune system attacking healthy tissues.
Metabolic syndrome and obesity. Excess fat tissue, especially visceral fat, produces inflammatory molecules (cytokines).
Diabetes. Insulin resistance and high blood sugar levels promote inflammation.
Heart disease. Chronic inflammation is implicated in atherosclerosis and other cardiovascular conditions.
Recurrent injuries and the incomplete healing of old injuries.
Chronic pain. Conditions like fibromyalgia or osteoarthritis can cause inflammatory responses to persist.
Family history, including genetic predispositions to inflammatory or autoimmune conditions.
Epigenetic changes. Environmental and lifestyle factors can alter gene expression, influencing inflammation.
Allergies or food sensitivities. Chronic exposure to allergens or intolerances (e.g., gluten or dairy) can trigger inflammation.
Chronic inflammatory diseases are in a category all their own, like inflammatory bowel disease (IBD), psoriasis, or chronic sinusitis.
Approaches to Managing Inflammation
Managing inflammation isn’t one-size-fits-all. Filtering approaches through your CREECS method (Cost, Risk, Effort, Effectiveness, Commitment, and Support) and aligning them with your personal health philosophy
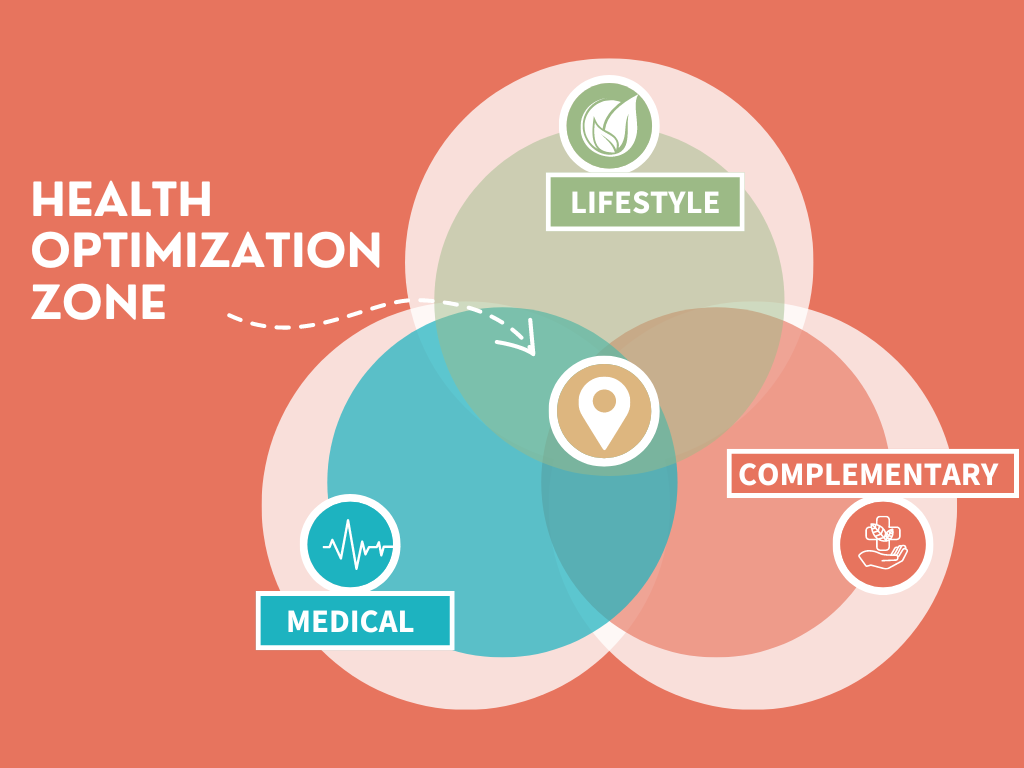
Whether you lean toward holistic methods, lifestyle changes, or a combination of medical and natural interventions, what matters is aligning with your values and beliefs. (This is what I’m referring to when I mention health philosophy, and it also speaks to what I call ‘The Health Optimization Zone’ — it helps you find harmony within medical, lifestyle, and complementary interventions.)
I created a cheat sheet to help you get started on addressing inflammation. Think of this as a starting point — if you aim to uncover the root cause of your health issue, you’ll find additional resources at the end of this post. Let this guide inspire you to dive deeper and do your research!
Inflammation Cheat Sheet
What You Need to Know and Do
Inflammation may be the body’s way of throwing a biological tantrum, but that doesn’t mean you must let it run the show. By understanding what sparks your body’s inner drama—be it sugar, stress, or the occasional love affair with processed foods—you can start to calm the flames.
Remember, there’s no one-size-fits-all approach; whether you tackle it with turmeric, meditation, or simply swapping fries for a salad (most of the time), you’re in charge.
Prioritize the Core 4, seek balance, and choose interventions that align with your health philosophy.
Think of inflammation as your body’s overly enthusiastic alarm system. It’s there to protect you, but sometimes it needs a gentle nudge—or a full reset—not to go off at every little thing. With a bit of strategy, a dose of self-awareness, and maybe a pinch of anti-inflammatory herbs, you can restore balance and get back to feeling like the best version of yourself.
So, what can you do about it?
I created a guide for this exact reason. You can find it here at the download link!
You can also find a health coach to help you narrow down your symptoms and options—and, of course, my comments section and DMs are always open. I’m happy to help you manage the next steps… that’s what I’m here for!
Alright, that’s all for today’s inflammatory talk. :) Let me know what you think in the comments!
In good health,
Dr. Alice
A little more about Dr. Alice Burron and The Health Navigator Group:
You can find more about The Health Navigator Group at our website: www.thehealthnavigator.org
On Instagram: @the.health.navigator
And learn more about Dr. Alice Burron at her website: draliceburron.com
Or via her personal Instagram: @dr_burron
You can even connect with her on LinkedIn, if you want to be professional about it. 👓
And if you’re not subscribed to our Substack, what are ya doing? It’s free, and packed full of useful tools to help you on your journey to better, faster healing.