Happy Thursday, health heroes!
Today, we’re talking about a very inflammatory topic. (No, not my post about Make America Healthy Again — nice try.)
I’m talking about literal inflammation. You might feel it in your joints, bowels, skin… or just about anywhere, really. So, what does it mean? And how can you treat it?
We all know that one person with an inflammatory personality—the one who walks into a room and, within minutes, manages to stir up drama like a storm cloud. Interestingly, physical inflammation behaves in much the same way. It’s the body’s version of overreacting, sounding the alarm at the slightest hint of trouble and summoning an immune army to swarm the scene.
This response is helpful when needed, like warding off infections or healing an injury. But when it overstays its welcome, just like that drama-loving friend, it can irritate everything in its path and cause more harm than good. Chronic inflammation turns this beneficial process into an unwelcome guest, disrupting peace and balance in the body. The result can be chronic pain, fatigue, and a whole host of other problems. Most of them can be avoided by knowing what inflammation is, and how to counter it.
Let’s break down inflammation into its subparts so you can see how it starts, how to recognize it, and what steps you can take to manage it.
What is inflammation, anyway?
Inflammation is the body’s natural defense mechanism triggered by injury, infection, or harmful stimuli.
It’s part of the immune response designed to isolate and heal affected tissues. However, when inflammation becomes chronic, it can lead to various health issues and contribute to long-term damage.
🕯️ Acute inflammation is a short-term response, like swelling after an ankle sprain. It’s generally beneficial and part of the healing process.
🔥 Chronic inflammation, on the other hand, persists over time and may become harmful, contributing to conditions such as arthritis, high blood pressure, cardiovascular disease, diabetes, and autoimmune disorders.
Short-term inflammation is good, but long-term inflammation is not good.
How Inflammation Begins and Where it Ends.
At the cellular level, inflammation starts when tissues are damaged, or pathogens (organisms that use us as a host and cause disease) are detected. The immune system responds by releasing inflammatory markers such as cytokines, which signal white blood cells to the area.
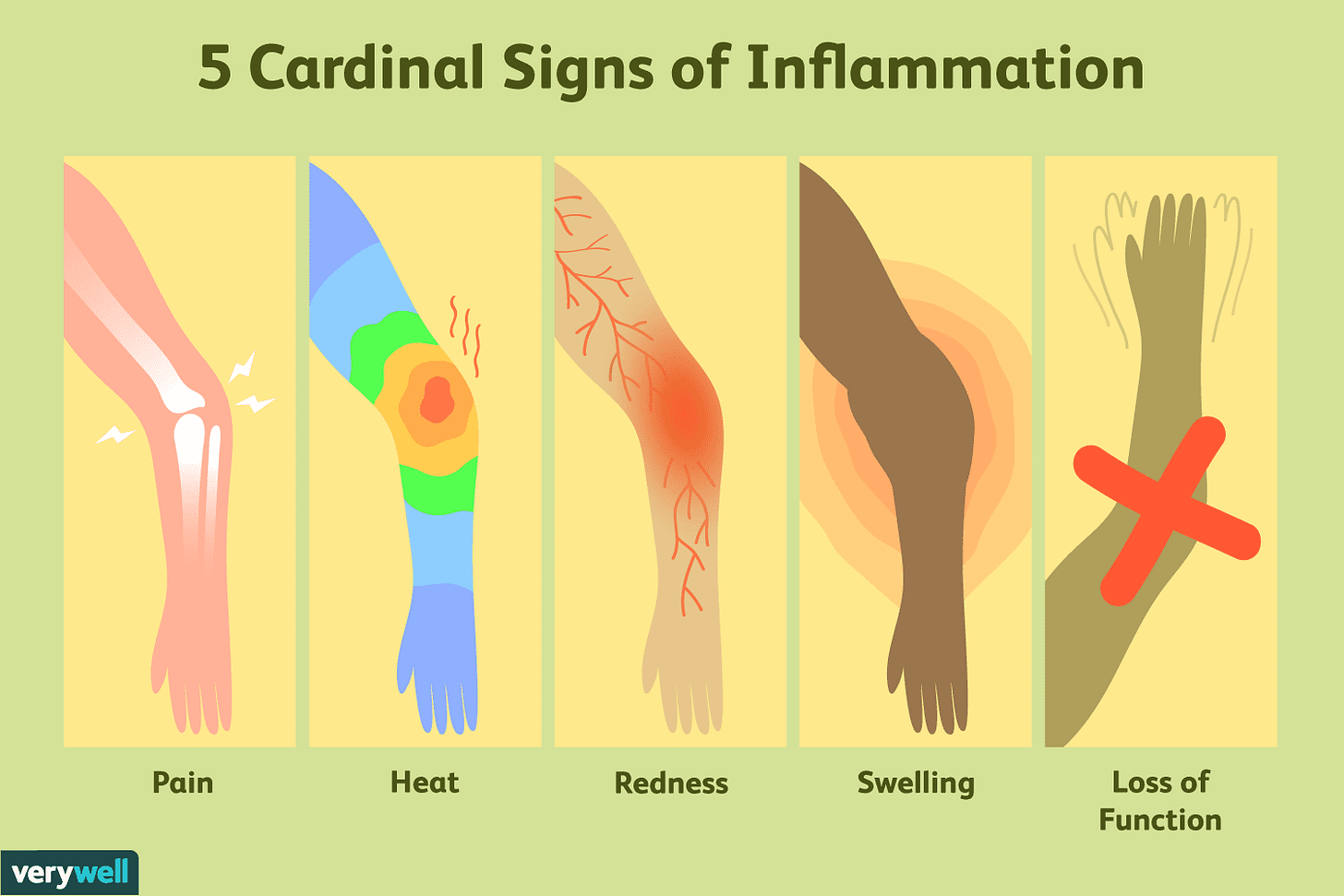
This cascade increases blood flow, resulting in redness, heat, swelling, and sometimes pain.
Symptoms and Signs of Inflammation
First, it’s important to note the difference between symptoms and signs.
😓 Symptoms are subjective experiences that can’t be measured, like how you feel, such as fatigue, joint stiffness, or feeling generally unwell.
🩸 Signs are measurable, including high blood pressure, elevated C-reactive protein (CRP) levels, or abnormal blood sugar readings.
It’s easier for doctors to base their treatment decisions on signs and less so on symptoms.
This is because there are medications and treatments that address signs, not symptoms, that doctors can pull out of their arsenal. That is why doctors have such a hard time with hard-to-describe health symptoms – there are seldom treatment interventions in their toolbox for many symptoms, so targeting inflammation and pain is often the approach.
This is one reason why opioids were prescribed for pain—it masks all kinds of symptomatic pain.
An example of a symptom for which doctors often lack effective treatments is chronic fatigue. It’s nonspecific, varies widely among individuals, and can stem from multiple overlapping causes, such as stress, hormonal imbalances, or post-viral syndromes.
While conventional medicine may address the signs indicating underlying conditions like anemia or sleep disorders, it often falls short in treating idiopathic or multifactorial fatigue. But if someone has a symptom of fatigue and has their thyroid checked and blood work indicates hypothyroidism, then that’s a sign, and that can be treated with medical interventions, such as medication.
Chronic inflammation can be subtle and creeps up over time, sometimes showing up as:
Persistent fatigue or low energy
Unexplained body aches or joint pain
Digestive issues, like bloating or irregular bowel movements
Skin problems, such as rashes or acne
The Role of Stress and Lifestyle
Stress plays a significant role in inflammation. Chronic stress triggers the release of cortisol, which, in high and prolonged amounts, can increase inflammation. This is compounded by lifestyle factors in the U.S., where diets rich in processed foods, sedentary habits, and lack of sleep are common.
Foundational methods for controlling chronic inflammation
To manage and reduce inflammation, always start with what I call the Core 4 nutrition, exercise, sleep, and hydration. (You can read more about why the Core 4 is so powerful in nurturing good health here — it’s one of the founding principles here at The Health Navigator.)
🫛 Nutrition.
Shift to an anti-inflammatory diet rich in vegetables, fruits, lean proteins, and omega-3 fatty acids. Limit processed foods and trans fats. I have to stop and park on the topic of sugar for a minute.
When we consume sugar, it’s quickly broken down into glucose and absorbed into the bloodstream, causing blood sugar levels to spike. In response, the pancreas releases insulin, a hormone that helps cells absorb glucose for energy or storage. Occasional sugar intake isn’t a problem for most people, but excessive sugar consumption can lead to several inflammatory processe.
Repeated blood sugar spikes stimulate the body to produce more insulin. Over time, this can lead to insulin resistance, a state where cells become less responsive to insulin. This condition often triggers chronic, low-grade inflammation as the body struggles to manage glucose effectively.
Excessive sugar in the blood can bind to proteins and fats, forming harmful compounds called Advanced Glycation End Products, or AGEs. These compounds damage cells and tissues and activate inflammatory pathways.
High sugar intake promotes fat accumulation, particularly visceral fat (fat stored around the organs), which secretes inflammatory substances known as cytokines.
While sugar is a major culprit, other foods and dietary patterns can also trigger inflammation:
Refined carbohydrates. Foods made from white flour, such as bread, pastries, and certain cereals, can cause similar blood sugar spikes and insulin responses as sugar.
Trans fats. Found in partially hydrogenated oils and processed foods like baked goods and margarine, trans fats can increase inflammatory markers in the body.
Fried and processed foods. These foods often contain high levels of advanced glycation end products (AGEs) formed when food is cooked at high temperatures. AGEs trigger inflammation by binding to specific cell receptors and initiating an immune response.
Red and processed meats. These meats can contain high levels of saturated fats and other compounds that promote inflammation.
Excessive alcohol. Chronic alcohol consumption disrupts the gut barrier, allowing bacteria to pass into the bloodstream and trigger inflammatory responses.
How Does This Work at the Cellular Level?
At the cellular level, the consumption of these inflammatory foods activates pathways that lead to the production of pro-inflammatory cytokines. When these substances are released, immune cells respond, setting off a chain reaction that can lead to chronic inflammation if exposure is consistent. Inflammatory markers such as C-reactive protein (CRP) and interleukin-6 (IL-6) are often elevated when the body is under this type of stress.
To combat inflammation, prioritize a diet rich in whole, anti-inflammatory foods like leafy greens, berries, fatty fish (rich in omega-3 fatty acids), nuts, and olive oil. A Mediterranean diet is a great place to go for ideas on how to eat to reduce inflammation. Reducing the intake of refined sugars and processed foods will also keep inflammation at bay and support overall health.
🏃♂️Exercise.
Your body was built to move. Movement induced by our muscles pushes blood to the muscles and joints and lubricates joints. It circulates inflammatory compounds in the body so that they can be taken from muscles and joints and released into our blood to be shuttled away. But think of exercise as a therapy – don’t lift heavy weights and run sprints or long distances if you’re trying to reduce inflammation. Exercise causes some stress and inflammation, so incorporate gentle and restorative exercise into your routine if you’re inflamed. Gentle walking, stretching, and strength training are great places to start.
💦 Hydration.
Water helps your body move blood filled with inflammatory compounds out and supports other organs and systems in the body, which will, in turn, manage inflammation.
🛏️ Sleep.
When we sleep, we heal and repair. Growth hormone gets a chance to rise and restore injuries. Sleep also allows our immune system to fight off pathogens, and it even reduces stress, which causes inflammation.
Whew! That’s already a lot of info.
There’s more to be said about inflammation — I’m going to continue on this thread next week with an inflammation cheat sheet to help you figure out what you can do about it!
See you Tuesday, health heroes.
Dr. Alice
(*Edit: The first email version of this email said it was Tuesday, not Thursday… luckily we’re a lot closer to Friday than I thought!)
A little more about Dr. Alice Burron and The Health Navigator Group:
You can find more about The Health Navigator Group at our website: www.thehealthnavigator.org
On Instagram: @the.health.navigator
And learn more about Dr. Alice Burron at her website: draliceburron.com
Or via her personal Instagram: @dr_burron
You can even connect with her on LinkedIn, if you want to be professional about it. 👓
And if you’re not subscribed to our Substack, what are ya doing? It’s free, and packed full of useful tools to help you on your journey to better, faster healing.