A Pill for Exercise? Exercise Mimetics are Coming, So Be Prepared.
Also, a chance to vote on my upcoming book cover!
Hello, health heroes.
We’re forecasting into the near future today, a future that sounds like sci-fi, but is our new reality.
But first, a very important question for you all:
Which book cover do you like better?
As you know by now, my new book will be arriving in May! This is the fun part. I’ve whittled it down to the top two cover options, but I need your help.
This poll is only live through the end of the week, so please let me know what you think!
Ok, now let's dive into an almost unbelievable futuristic new landscape today. Prepare yourselves by reading this article because otherwise, you won’t be ready for the future. Hang on to your hats. You’re not going to believe this.
Let’s talk about the future.
In the coming years, we’ll face a tidal wave of medical breakthroughs offering new opportunities to intervene in our health. From medications designed to mimic the effects of exercise to therapies targeting inflammation to suppressing Alzheimer’s disease and beyond, the biotech and pharmaceutical industries are racing to bring innovations to market.
While these advances hold tremendous promise, they also present a challenge: how can individuals make sense of it all? When we’re offered a new medication, should we jump up and gladly take it, or should we think twice, knowing there are always consequences when we do and when we don’t?
Exercise Mimetics: A Case Study in Complexity
Imagine taking a pill that mimics the effects of a 30-minute workout. Well, it’s coming, folks.
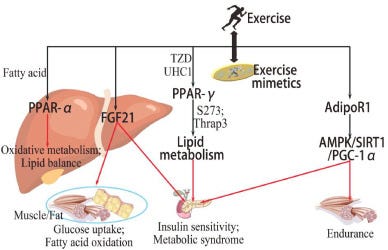
This is a medical induction of exercise mimetics, a way to mimic the effects of exercise via a pill.
That’s right – this is no longer the stuff of science fiction. It’s on its way, maybe in as little as three to five years. Researchers are developing medications that activate the same pathways triggered by physical activity, improving cardiovascular health, muscle strength, and metabolism without requiring you to lace up your sneakers.
As an exercise physiologist, I must admit that I found the idea of exercise mimetics appalling at first. After years of training and studying athletes who worked grueling hours to achieve peak performance, it seemed irreverent to induce exercise-like effects with a pill, bypassing the effort and discipline required to build true physical fitness. However, the more I considered it, the more I realized that some practices already induce exercise-like conditions in the body without actual exercise. Sitting in a sauna, for example, raises heart rate, body temperature, and even blood pressure. It mimics aspects of exercise in a controlled environment. Similarly, other activities like cold exposure, vibration therapy, or even hypoxia training simulate certain physiological responses typically elicited by physical exertion.
The idea of exercise mimetics isn’t as far-fetched when we look at these examples. Yet, what’s critical to understand is that these approaches—and any potential medication—only induce some exercise-like responses, not all. Exercise does more than elevate heart rate or burn calories; it improves oxygen saturation, lung capacity, coordination, mental clarity, pain tolerance, mind-body synchronization, and reflexes. None of these responses are fully elicited by mimetics or passive interventions. No pill, therapy, or mimetic can replace the holistic benefits of physical activity. They are tools—not substitutes.
The promise of taking a pill to mimic exercise responses, especially muscle-building, is undeniably enticing, particularly for individuals with physical limitations or those at high risk for chronic disease.
This is even more relevant in light of the muscle-atrophying side effects of popular weight-loss medications like GLP-1 receptor agonists and GIPs (glucose-dependent insulinotropic polypeptide) agonists like Wegovy (Ozempic for diabetics) and Zepbound, as well as future combination therapies.
Groundbreaking technology or a new quick-fix?
For those with severe physical restrictions—such as individuals with disabilities, chronic illnesses, or extreme frailty—exercise mimetics may offer a lifeline to preserve muscle, improve metabolic health, and reduce the risk of further complications. For these individuals, such medications represent a groundbreaking advancement in their ability to maintain a baseline of health and functionality.
However, for the broader population, turning to a pill to induce exercise effects without actual exercise raises significant concerns. For one, the public may misunderstand what these medications can and cannot do, expecting them to replicate all the benefits of exercise. They won’t—and likely never will.
Moreover, medications like these risk creating a cycle of dependency or disincentivizing actual exercise, which provides unique and irreplaceable benefits, including improved mental health, bone density, balance, and resilience. And let’s not forget the potential for underground markets to emerge, offering unregulated versions of these drugs to those who don’t meet medical criteria for access.
The public’s desire for quick fixes often outpaces medical oversight.
This is where healthcare professionals, especially physicians, have an opportunity—and a responsibility—to think outside the medication box.
Rather than prescribing pill after pill to counteract the side effects of other medications, they can take a more holistic approach. For patients on GLP-1 medications, physicians can emphasize incorporating practices like resistance training and aerobic exercise, or at the very least, sauna therapy and cold exposure may be less costly and accessible ways to mitigate muscle atrophy and support overall health. These interventions not only address the root issue but also offer benefits that no pill can replicate, such as improved coordination, mind-body connection, and functional strength.
Exercise mimetics, like other emerging innovations, offers a fascinating glimpse into how science is exploring new ways to support weight management and overall health. However, new products emerge every day, like bioactive peptides and polyphenols, representing another tier of intervention for individuals seeking a boost.
While these approaches may provide a helpful nudge, they are not replacements for the proven, long-term benefits of actual physical activity and a balanced diet.
Instead, they should be viewed as complementary tools, offering individuals an entry point into healthier habits or an additional option for those facing physical or metabolic limitations. The goal is to balance these advancements with tried-and-true strategies, creating a more inclusive and sustainable path to well-being.
By advocating for natural, accessible strategies alongside medical therapies, healthcare providers can empower patients to reclaim their health in a more balanced, sustainable way. Exercise mimetics and other medical advancements may play a role in health management, but they should never overshadow the unparalleled value of real physical activity and complementary interventions.
At the same time, we must not dismiss the individuals for whom these innovations could be life-changing, offering them an opportunity to reclaim some of the health and mobility that may otherwise feel out of reach. The future of health lies not in replacing exercise but in encouraging smarter, more integrated approaches to achieving well-being.
Exercise mimetics is just one example of the broader trend in pharmaceutical innovation. Fueled by venture capital and deep-pocketed investors, the biotech industry is accelerating research into therapies that aim to combat disease and improve quality of life.
These medications are also aimed at counteracting the muscle-wasting side effects of weight loss medications, such as GLP-1s. When these medications pass FDA trials, they quickly become part of the clinical toolkit, presented to patients as the next big breakthrough.
But with these innovations should come critical questions:
What would I gain versus losing if I took these medications?
Could I start moving more every day and get the same benefit without medication?
What are the risks versus benefits?
Given my goals, how long would I take the medication?
What are the side effects, and would I need medication to counter those?
How much am I willing to pay for these medications?
How might this alter my behavior over both the short term and long term?
To navigate these complex decisions, we need more than enthusiasm for breakthroughs—we need a roadmap. Once our doctors offer these medications, we need to be prepared and ready to think through the nuances. We must empower ourselves with truth and clarity before we are tempted to jump on the latest pharmaceutical intervention. We must be proactive. (Shameless plug - my upcoming book, Health Shift: Your Personalized Guide to Making Strategic Health Decisions, is that roadmap, and I can’t wait to get this into people’s hands to help them be proactive.)
On Thursday, I’ll share my three essential tools for health decision-making. They’re free and simple and require only that you consider your approach to health. If you have these tools, you absolutely can objectively navigate the tempting latest quick-fix approaches to your health, guaranteed. You won’t want to leave home without them.
See you Thursday with more good stuff,
Dr. Alice
⭐ ALSO — Please cast your vote for the book cover! I’d love to know what you think!
A little more about Dr. Alice Burron and The Health Navigator Group:
You can find more about The Health Navigator Group at our website: www.thehealthnavigator.org
On Instagram: @the.health.navigator
And learn more about Dr. Alice Burron at her website: draliceburron.com
Or via her personal Instagram: @dr_burron
You can even connect with her on LinkedIn, if you want to be professional about it. 👓
And if you’re not subscribed to our Substack, what are ya doing? It’s free, and packed full of useful tools to help you on your journey to better, faster healing.