The Medication Hype Cycle: Are We Missing the Bigger Picture in Health?
Both individuals and organizations are scrambling to understand their role in navigating the health hype cycle. Let's get to the bottom of it.
Medications like GLP-1s—Wegovy and Saxenda—are dominating conversations about health, particularly weight loss. Headlines call them “game-changers” for managing obesity, which is now considered a disease, and prescriptions are skyrocketing. But is this the whole story? Are these drugs a breakthrough, or are we repeating a familiar pattern in healthcare?
History suggests we may be caught in a hype cycle, a concept often used in technology to describe the rise, peak, and recalibration of expectations around innovation. A recent conference I attended with Harvard’s Dr. Gabbay reintroduced this concept in light of medications. This cycle is now playing out with medications, leaving both individuals and organizations scrambling to understand their role in navigating it.
The Rise of the Hype Cycle in Medications
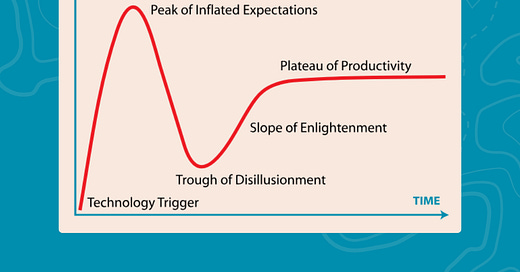
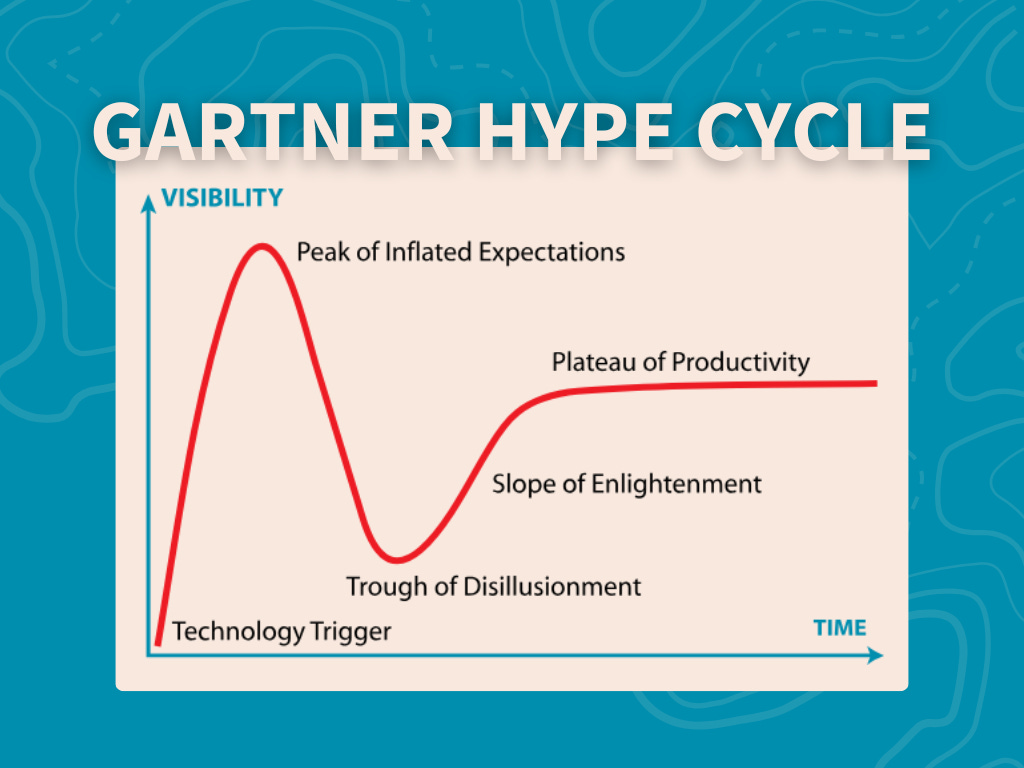
The Gartner Hype Cycle teaches us that every innovation goes through predictable phases:
The Innovation Trigger: A new drug emerges, supported by compelling science and marketed as revolutionary.
The Peak of Inflated Expectations: Media buzz, social validation, and rapid adoption create sky-high demand.
The Trough of Disillusionment: Side effects, costs, and unmet expectations lead to backlash and recalibration.
The Slope of Enlightenment: Evidence-based insights bring clarity about appropriate use.
The Plateau of Productivity: The drug finds its rightful place in healthcare, integrated with realistic expectations.
GLP-1s are now near the Peak of Inflated Expectations. They promise transformative weight loss and improved health, but the realities of cost, adherence, and sustainability are starting to emerge. So, what happens when the hype fades? And more importantly, what are we doing to prepare for it?
Personal Encounters: Stories from the Front Lines of the Hype Cycle
Sometimes, the most eye-opening insights don’t come from a conference presentation or a research paper—they come from conversations.
On my flight to Boston to speak at the Obesity and Metabolic Innovation Forum, I sat next to a woman who was taking Wegovy. She had experienced significant weight loss and was hopeful about the future. What stood out, though, was that she wasn’t navigating this journey alone. She had a healthcare team—a coach, exercise physiologist, dietitian, mental health provider, and a support group—all working together to ensure her success.
But then she shared another story, one that gave me pause. She mentioned a coworker who was actively trying to develop Type 2 diabetes just to qualify for insurance coverage of weight-loss medications.
This is a startling reflection of how our healthcare system sometimes incentivizes disease management over prevention. And, as she noted, even if this person succeeded in their misguided effort, insurance coverage for these drugs might still be uncertain because of differing dosage requirements for weight loss versus diabetes.
On the return flight, I met another woman who leaned over as I worked on this article. She had struggled with her weight for years and admitted she was tempted to try these new medications but held to a lifestyle-first philosophy. Yet, despite her belief in lifestyle changes, she wasn’t implementing them. Trauma in her life had derailed her efforts, and she felt stuck. What she really needed, she said, was support—a health coach or someone to guide her through sustainable changes. By the end of our two-hour conversation, she left inspired and ready to take ownership of her health.
These conversations left me with mixed emotions—hope for those using medications responsibly and frustration at how easily our culture and healthcare system seem to push quick fixes over comprehensive support. Just this week, I walked into my dermatologist’s office and saw an ad for semaglutide and tirzepatide injections offered through a medspa partnership. There was no mention of concurrent lifestyle support.
This is part of the problem. GLP-1s are being offered everywhere now, even in places without the infrastructure to provide the kind of coaching, guidance, and behavioral support that ensures long-term success. People are being set up to believe that medications alone will solve their health challenges. But what happens when the medication stops?
The stakes feel even higher when I hear stories like my client’s sister, who is losing weight on Wegovy without making any lifestyle changes at all—just sitting on the couch. Without addressing the root causes of obesity, the weight will almost certainly return. And that’s the heart of the issue: Are we really helping people achieve health, or just creating another cycle of dependency?
These experiences illustrate how the Hype Cycle of medications isn’t just a theoretical framework—it’s playing out in real-time. And as we hurtle forward, introducing more innovative medications and new promises of transformation, we must ask: What are we doing to address the root causes of health issues? How can we support individuals in a way that sustains their success, whether or not they choose to use medication?
We can’t afford to keep neglecting prevention, lifestyle support, and the daily choices that ultimately determine long-term health. If we want to break this cycle, we must focus on education, advocacy, and a broader view of health—one that empowers individuals and organizations to work together for lasting change.
Beyond Medications
This isn’t just about GLP-1s. The cycle of hype applies to every “cure-all” medication, trendy diet, or supplement that captures public attention. It reflects a deeper cultural issue: our tendency to view health as something external—a problem solved by innovation and the latest approach, not by daily actions.
Yes, we are victims to some extent. Our environments are saturated with ultra-processed foods, sedentary lifestyles, and marketing that prioritizes convenience over well-being. But we’re also fooling ourselves if we think a single medication is the answer. Health is not a one-time decision; it’s the result of thousands of small, daily choices. Medications can support health, but they can’t replace the basics—nutrition, movement, sleep, and hydration. Nor can they create mental resilience.
The Individual’s Role: Holding the Cards
As individuals, we hold more power than we realize. Health literacy and advocacy are the keys to navigating this pro-medication, anti-health culture. When we understand the trade-offs, ask the right questions, and make informed decisions, we shift the balance of power back to us. You and I get to decide if we are medication-first, or we are willing to do the work to get healthier.
What does that look like in practice? It means viewing medications like GLP-1s as tools, not solutions. It means integrating them into a broader plan that includes diet, movement, and behavioral support. And it means demanding better from our healthcare system—not just access to drugs, but access to education, prevention, and support for lasting change.
For Organizations: The Cost of Ignoring Prevention
For employers, payors, and policymakers, the focus on disease management over prevention is short-sighted. Covering medications without addressing lifestyle factors creates a revolving door: temporary results followed by recurring costs. True cost containment comes from investing in comprehensive strategies that integrate prevention, behavior change, and treatment.
Looking Ahead: What’s Next?
What happens when the next medication comes along, promising even more miraculous results? Are we prepared for the ongoing cycle of inflated expectations and disillusionment? Or can we take a broader, more sustainable approach to health—one that balances innovation with wisdom and equips individuals to thrive in a complex health landscape?
The challenge for all of us—whether as individuals, employers, or healthcare leaders—is to step back and see the bigger picture. How can we reclaim our health in a world increasingly driven by quick fixes?
How can we use innovation wisely without losing sight of the basics? These are the questions we need to ask as we navigate the next phase of the hype cycle.
A Call to Action: Building a Community for Change
This is a pivotal moment. We are at a crossroads where innovation and hype dominate the conversation, but the deeper work of prevention, education, and sustainable health practices is still lagging behind. I know I’m not the only one who feels this tension. Many of you reading this—whether you’re a healthcare provider, an employer, a policymaker, or someone simply passionate about health—share the same concerns.
I believe we can do better, but I also know I can’t do it alone. This is a call to action for anyone who believes in empowering individuals to take ownership of their health, promoting health literacy, and creating systems that support sustainable, meaningful change.
If this resonates with you, I invite you to join me. Let’s build a community—a tribe—of like-minded individuals and organizations who are ready to take on this challenge together. Whether you’re already working in this space or just starting to explore how you can make a difference, there’s room for your voice, your expertise, and your passion.
If you’re ready to join this conversation or collaborate on solutions, connect with me here on LinkedIn or reach out directly. Together, we can amplify this message and create real change.