Special Edition: The Core 4: Sleep
This overlooked pillar might be the missing piece in your health equation.
I used to be one of those lucky people who could fall asleep the minute my head hit the pillow. I never gave it much thought—sleep just happened. It wasn’t until menopause arrived, seemingly overnight, that sleep became a mystery I couldn’t solve. I’d fall asleep easily, only to wake up a few hours later, wide-eyed and restless. My body felt tired, but my brain was stuck in overdrive. Sound familiar?
The change in my sleep pattern sparked my curiosity. Why did sleep—something so effortless for decades—suddenly unravel? And more importantly, what was it doing to my health? The deeper I dove into the science of sleep, the more fascinated I became. I soon realized: if you don’t have sleep, you don’t have a stable foundation for healing or health.
That’s why sleep is a non-negotiable in the Core 4. It’s not just another “wellness thing.” It’s the biological permission slip for everything else your body needs to do well—repair, regenerate, regulate, remember, and even imagine.
Let’s dig into why sleep might just be the most undervalued vital sign in our modern world.
This is another special Wednesday edition in our dive into the Core 4. If you’re new here, Health Shift is typically published on Tuesdays and Thursdays... but I added an extra Wednesday Special Edition to encompass the Core 4. We’ll be referencing them often, and they are foundational to health and healing. This is the last one in the series of 4.
You can catch up on the previous pieces about the Core 4 here:
How Sleep Impacts Our Physiology
I began to wonder how sleep impacted every part of the body. As I studied each physiological system and its impact on it, I quickly discovered how sleep is intricately involved and entwined to nearly every system in the body.
Let’s examine a few of our systems and the impact of sleep to provide some examples.
🧠 Nervous System
During deep sleep and REM cycles, your nervous system gets to hit the “reset” button. The parasympathetic system (the rest-and-digest branch) takes over, reducing inflammation, lowering heart rate, and repairing stress-induced wear and tear.
Without enough restorative sleep, the sympathetic system (also known as the fight-or-flight response) remains on standby, much like an overcaffeinated bodyguard, making it harder to relax even when you want to.
Sleep also clears neurotoxins from the brain through the glymphatic system, a network of vessels in the brain that plays a crucial role in clearing waste products and toxins from the central nervous system.
Poor sleep means more junk is left behind, more brain fog, and even potential links to neurodegenerative conditions.
🌿 Gut Health
Our gut has its own circadian rhythm. Disrupted sleep throws off the timing of digestion, absorption, and even the production of neurotransmitters like serotonin, which regulates both mood and melatonin production.
An unhappy gut can lead to an unhappy brain—and vice versa.
🛡️ Immune System
Sleep is like a nightly boot camp for your immune cells. During sleep, your body increases the production of cytokines—proteins that target infections and inflammation.
One night of poor sleep reduces the effectiveness of your natural killer cells by nearly 70%. Think about that the next time you feel a cold coming on after a rough night.
Cellular Consequences: The Microscopic Toll
On a cellular level, sleep facilitates chemical processes within your cells, helping to mitigate inflammation and metabolic dysfunction, among other benefits.
We determine this by examining biomarkers in the blood. For example…
Inflammation: Sleep loss is characterized by an increase in circulating proinflammatory cytokines (IL-1β, IL-6, IL-17A, TNF-α) and C-reactive protein (CRP), leading to a chronic inflammatory state.
Metabolic Dysfunction: Sleep deprivation impairs glucose metabolism and insulin sensitivity, increasing the risk of type 2 diabetes.
Sleep is no joke - it’s actually powerful medicine.
What About Sleep Supplements?
We’re living in a culture that wants to buy sleep.
Between melatonin gummies, magnesium sprays, and prescription sleep aids, the market is booming. But here’s the catch: while some of these options can help you fall asleep faster, they don’t always help you get better sleep.
In fact, studies show that certain sleeping pills (especially those in the benzodiazepine class) may reduce the time it takes to fall asleep—but they also reduce the amount of time spent in deep and REM sleep, the phases responsible for memory consolidation, emotional processing, and creativity.
And melatonin? It can be helpful for circadian rhythm issues like jet lag or shift work—but many people take it inappropriately or at doses far too high. Plus, it’s a hormone. Repeated use can actually suppress your body’s natural production over time.
If you've ever woken up feeling “drugged” after taking a sleep aid, that's your brain telling you it didn’t get the kind of sleep it needed—just sleep that was artificially induced.
The Creative Brain: Sleep’s Surprising Superpower
Ever woken up with a new idea? A solution to a problem you couldn’t solve the night before? A song in your head out of nowhere?
That’s not a coincidence. REM sleep is the stage where our brains play with connections, test ideas, and stir up creativity. It’s where our subconscious finally gets to take the wheel.
Some of history’s greatest scientific and artistic breakthroughs were credited to dreams or early morning clarity.
Sleep isn't just passive. It's where your brain actively works through problems, encodes memories, and sows the seeds of your future ideas.
So, When Should You Worry?
If you're consistently struggling with:
Loud snoring, gasping, or choking at night
Morning headaches or dry mouth
Daytime sleepiness even after “a full night’s sleep”
Memory or focus issues
Mood swings or increased anxiety
High blood pressure or irregular heartbeat
…a sleep study may be your best next step.
Most people don’t realize these are signs of sleep-disordered breathing—especially obstructive sleep apnea. This condition affects millions and often goes undiagnosed.
A sleep study (often covered by insurance with a referral) can be done at home or in a sleep lab, and it could change your life.
🌙 What About Naps?
Naps can be a strategic move if you’re not getting enough sleep at night. But the secret is in the duration:
10–20 minutes: Boosts alertness and mood
30–60 minutes: Can lead to grogginess (sleep inertia)
90 minutes: Full sleep cycle, helpful if you’re sleep-deprived
Avoid napping too late in the day, and if you’re napping regularly but still tired, that’s a clue something deeper is off. (Like, maybe it’s time for that sleep study…)
Sleep Across Our Lifespan
Our sleep requirements evolve with age, so it’s essential to recognize that our sleep needs change throughout our lives. Sleep needs ebb and flow with our age and activity level. It’s not an exact science. Instead, think of it as balancing your body’s ever-changing needs to rest and recover.
Newborns (0-3 months): 14-17 hours per day.
Infants (4-11 months): 12-15 hours per day.
Toddlers (1-2 years): 11-14 hours per day.
Preschoolers (3-5 years): 10-13 hours per day.
School-age children (6-13 years): 9-11 hours per day.
Teenagers (14-17 years): 8-10 hours per day.
Adults (18-64 years): 7-9 hours per night.
Older Adults (65+ years): 7-8 hours per night.
As we age, sleep patterns change, with older adults experiencing lighter sleep and more frequent awakenings. Although we wish we could sleep like babies when we’re older, as our sleep patterns change, our expectations may also need to change.
Sleep and the Menopausal Mystery
It turns out I’m not alone when it comes to sleep disturbances and menopause. Sleep disruptions during perimenopause and menopause are incredibly common—and hormonal changes are largely to blame. As estrogen and progesterone levels drop, they take with them their calming, temperature-regulating, and sleep-promoting effects. Progesterone, in particular, has a sedative-like quality, and without it, many women find themselves waking up hot, anxious, and alert at 2:00 AM, wondering what just happened.
And let’s not forget cortisol. When sleep is fragmented or shortened, cortisol levels remain elevated for a more extended period. High cortisol not only interrupts deep sleep but also disrupts blood sugar and appetite regulation.
Barriers to Quality Sleep: Identifying the Culprits
Several factors can sabotage our slumber, and many are within our control. Consider how you can begin to control the variables within your control.
Lifestyle Choices: Irregular sleep schedules, excessive caffeine or alcohol intake, overeating or eating too late, and lack of physical activity can disrupt sleep. Try doing something with these variables — cutting out those energy drinks, maybe, or getting some movement can go a long way.
Work Habits: Sedentary jobs and non-traditional work schedules are associated with poor sleep quality. Can you incorporate more activities to see if they help you sleep better?
Stress and Anxiety: Elevated stress levels can interfere with the ability to fall and stay asleep. Can you try implementing stress management techniques, such as yoga, meditation, or listening to restful music, to improve your sleep?
Strategies for Restful Sleep
While some sleep disruptors are beyond our control (hello, full moon!), we can adopt habits to enhance sleep quality:
Consistent sleep schedule. Going to bed and waking up at the same time daily helps regulate your body's internal clock.
Create a restful environment. Keep your bedroom cool, dark, and quiet. Consider using earplugs or white noise machines to block out disturbances. And try not to work in the same place that you sleep, if you can help it. Your brain will associate a room for sleep with sleeping, not stress or emails.
Limit screen time before bed. The blue light emitted by phones and computers can interfere with melatonin production, making it harder to fall asleep.
Physical activity. Regular exercise can promote better sleep; however, avoid vigorous workouts close to bedtime. Even stretching or deep movement before going to bed can help. (Try looking up yoga for bed or yoga in bed — yes, it’s a thing.)
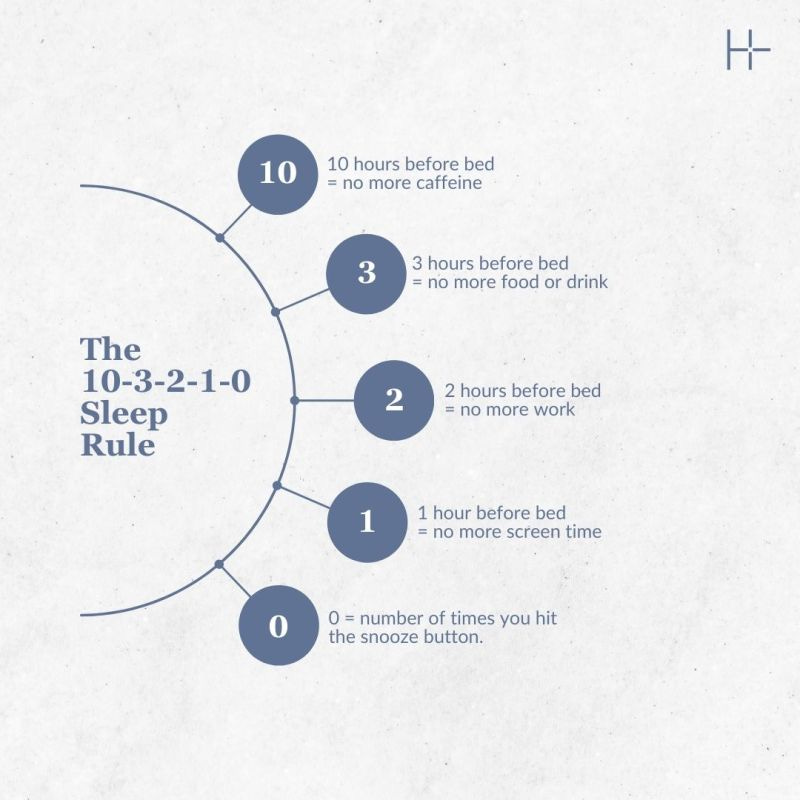
If you're not ready to dive into medical testing but know something has to change, start with this simple, science-backed routine:
10 hours before bed: Cut off caffeine
3 hours before bed: Stop eating or drinking alcohol
2 hours before bed: No more work
1 hour before bed: Shut down screens
0 times hitting snooze in the morning
It’s not a magic wand—but it’s a framework to retrain your circadian rhythm and signal safety and consistency to your nervous system.
And if you’re saying, “But Dr. Alice, life just doesn’t work like that! Sometimes I get home from work really late, and can’t do any of those things!” I hear you. Our world isn’t wired for us to get good, restful sleep.
Choosing to prioritize sleep — even a handful of better practices — can go a long way. It’s worth it.
Quality, Quantity, and Timing (AKA, The Sleep Triad)
Much like a balanced diet and the way I approach nutrition in the Core 4, optimal sleep hinges on three factors:
Quality: Deep, restorative sleep is crucial for physical and mental health.
Quantity: Adequate sleep duration varies by age but generally falls between 7-9 hours for adults, as I outlined previously.
Timing: Aligning sleep patterns with natural circadian rhythms enhances sleep quality. In other words, avoid going to bed too early or too late, and try to get most of your sleep at night, if possible, rather than during the day.
Your Employer Should Care About Your Sleep!
Yep, I said it. Poor sleep leads to disease. It would be wise for employers to consider helping employees get better sleep. Here are some other reasons why good sleep will benefit employers.
Employees who sleep well:
Make better decisions
Get sick less often
Are more creative
Have fewer workplace accidents
Are more productive (by a long shot)
Sleep isn’t a “perk.” It’s a performance enhancer. Just as nutrition education and stress management, sleep hygiene should be part of every workplace wellness program. I help organizations strategize sleep as a Core 4 strategy within their employee benefits. Ask your employer about your sleep benefits - you may have some perks waiting to help you sleep better.

A Vital, Beautiful Gift.
At its core, sleep is both an ancient biological necessity and a modern-day challenge. It’s influenced by everything—your hormones, your emotions, your habits, your history. And yet, much of it also in your control.
I now treat sleep like I treat the time I’m awake—with care, intention, and curiosity. It’s no longer an afterthought or something I’ll “catch up on” later. It’s part of my healing, my performance, and my peace.
So, whether you’re waking up at 3 AM sweating through menopause, scrolling past your bedtime, or trying to function after one too many sleepless nights—know this: better sleep is possible, and it doesn’t have to be perfect sleep. And it just might be the missing link in your journey to feel well, heal faster, and thrive.
Let’s start treating sleep like the powerhouse it is.
Because when sleep goes right, everything gets better.
A little more about Dr. Alice Burron and Strategic Action Health:
Dr. Burron is a co-founder of Strategic Action Health, dedicated to helping organizations help their employees make better health decisions. Come check us out here!
Catch us on Instagram: @the.health.navigator and @dr_burron
You can also connect on LinkedIn, if you want to be professional about it. 👓
And if you’re not subscribed to Health Shift here on Substack — it’s time! This free newsletter is packed with valuable information and approaches to help you on your journey to better, faster healing.
Health Shift: Your Strategic Guide to Making Strategic Health Decisions book will officially launch on May 17, 2025! Mark your calendars! And if you’re in Cheyenne, join us for our party at Blacktooth Brewery. Have a beer on us! More information is coming soon.