Running on Empty: When You Begin to Burn Out but Life Keeps Going
What to do about your burnout.
I’m sure you know the feeling: you’re barely keeping the plates spinning, your brain is stuck on spin cycle, your emotions are fried, and even walking across the room feels like a hike up Everest in a snowsuit.
And yet, your to-do list doesn’t care. Your job needs you. Your family needs you. Dinner needs to be cooked. While life goes on at the speed of light, you feel like you’re unintentionally slowing down.
I’m there right now. I’ve hit the point where high mental demand, ongoing problem solving, continual physical demand, and consistent stress are leaving me tired. My legs feel heavy. I wake up with two-thirds of a charged battery. I’m suddenly craving sugar, even though I eat clean. I feel like I’m gaining weight, even when the scale disagrees, because I’m simply bloated. My gut hurts, and my emotional perspective is more negative than positive. This is not just stress anymore. It’s stress in 4K Ultra HD, running 24/7 solutions to problems that don’t even exist.
I recognize the symptoms because I’ve been here before and recognize the signs. I want to share what exactly is happening in the body when emotional exhaustion shows up, such as physical fatigue, cravings, gut issues, and a feeling like you just don’t want to do this anymore.
It’s called burnout, and we all experience it at various stages of our lives, especially during life changes. If you haven’t thought about this before, you can benefit from recognizing the symptoms of emotional and physical burnout, so you know how to stay resilient. Join me in overcoming seasons of burnout. Let’s zoom in.
The Brain in Survival Mode
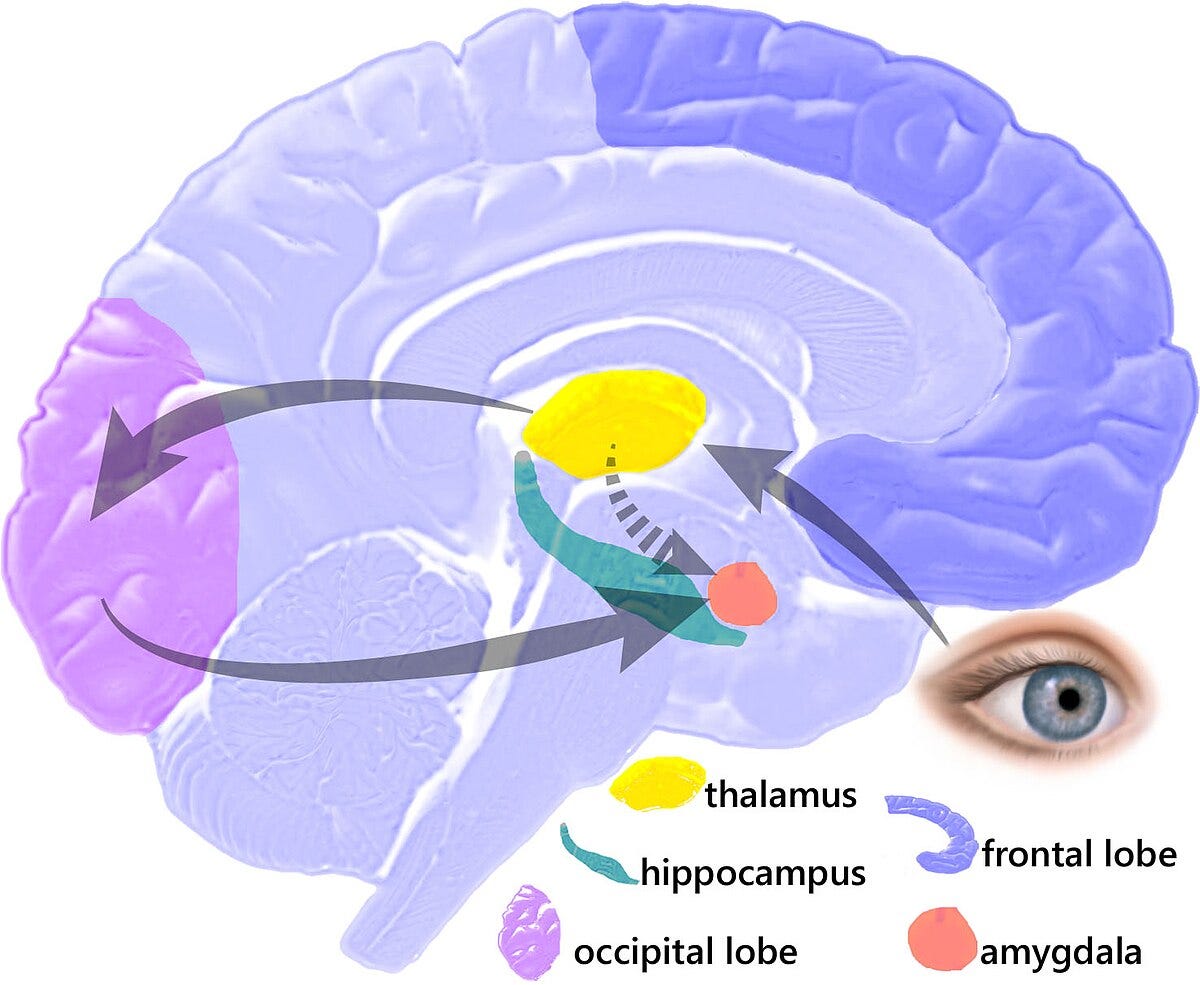
Stress isn't just a feeling; it’s a response, like a full-body alert system. When the brain perceives a threat (even an emotional one like conflict, grief, or financial pressure), the amygdala triggers the hypothalamus, which signals your sympathetic nervous system: Activate! Out comes the adrenaline. Cortisol. Epinephrine. The body readies for battle.
You may have heard it called an amygdala hijack, which is that moment when your brain flips into panic mode over something that isn’t actually life-threatening (like a tough email or a family crisis). What’s really happening behind the scenes is a full-on activation of the HPA axis—the hypothalamic–pituitary–adrenal system.
This is your body’s central stress response highway, sending signals from your brain to your adrenal glands to release stress hormones like cortisol and adrenaline. It’s a brilliant design for surviving life threats like when running for your life... but it’s a little less helpful for surviving a Tuesday.
But emotional threats are tricky. They don’t come with a sword and a deadline. They linger. They hide in replayed conversations, to-do lists, inboxes, bills, and 3 a.m. thoughts. So your body stays revved up far longer than it’s built for.
This constant activation:
Burns through glucose and glycogen, your brain’s primary fuels
Disrupts sleep and circadian rhythms
Suppresses the immune system
Interferes with digestion and hormone regulation
Triggers cravings for quick energy—hello sugar and carb cravings
It’s like keeping your foot on the gas pedal while your body begs for a rest stop. Eventually, even your mitochondria—the literal energy generators in your cells—start dialing it back. That’s when physical feelings like heaviness hit.
Why We Crave Sugar When We’re Stressed
Cortisol, released by the adrenal glands, and insulin, released by the pancreas, are hormones that play crucial roles in regulating blood sugar and energy metabolism but act in opposing ways.
Cortisol, released during stress, increases blood sugar levels to provide energy for the "fight or flight" response, while insulin helps cells absorb glucose to lower blood sugar.
When cortisol rises, insulin does too. Cortisol stimulates the release of glucose into the bloodstream, but cortisol also makes cells less responsive to insulin, meaning more sugar stays in your bloodstream longer. Chronic high cortisol levels can lead to insulin resistance and increased blood sugar levels over time. This is because the body becomes less sensitive to insulin, and the pancreas may not be able to produce enough insulin to keep blood sugar levels in check. Your brain interprets this as a shortage, and the cravings kick in.
Not to mention, your brain loves glucose. It’s like candy to a toddler—quick fuel, instant comfort. But it’s a trap. The sugar gives a short boost, then crashes you harder, leaving your body more depleted than before.
Another concern with high cortisol over time is that chronic stress can lead to elevated cortisol levels, contributing to muscle tension, inflammation, and even the exacerbation of pre-existing back conditions. This can create a cycle where stress and pain reinforce each other, making it a complex relationship.
The Hidden Toll of Pushing Through
Even when you eat well, sleep, move, and hydrate (hello, Core 4!), the load of emotional stress takes its toll. You might not collapse, but you’ll feel the weight. Have you ever felt like something was weighing heavily on you? It’s not just one thing; it’s probably everything, which is collectively releasing cortisol into your system.
If you keep working at full capacity while under emotional or physical cortisol siege—trying to be the hero at work, home, and life—your body will adapt... until it can’t. And everyone has a different capacity to handle this ongoing threat. But symptoms show up as:
Weight gain or loss
Loss or gain of appetite
Brain fog
Irritability or numbness
Physical fatigue that doesn’t resolve with rest
A feeling of being “toxic” or energetically heavy
Gut issues
Back pain
A case of the “I don’t care anymore-itis,” where your tendency to care decreases
Feeling like the life is sucked out of you
Becoming cynical about everything in general
If you’re experiencing these symptoms and have been stressed for weeks, not days, you will likely experience burnout.
So, What Can You Do to Refill the Tank?
If you’re feeling emotionally spent, motivation will not pull you out. Tenacity will not change anything. Gutting it out won’t overcome the exhaustion. What will? Restoration will.
Here’s a survival kit to start refilling, not just powering through:
1. Create Micro-Moments of Relief
Many tiny breaks = collective big returns. Step outside. Breathe slowly for 90 seconds. Do this over and over. Cry in the car (yes, that counts). Rebooting doesn't require a sabbatical; sometimes it starts with just 10 intentional minutes. Listen to calm music. Drink a cup of tea. Close your eyes and imagine you’re somewhere else. Journal.
2. Get Spiritual or Still
Whether it’s prayer, meditation, or just sitting in awe of a sunrise, moments of stillness reconnect us to something beyond the daily grind.
“Stillness is not the absence of movement or sound. It's not about focusing on nothingness but creating a physical and emotional clearing to allow ourselves to feel, think, dream, and question." Brené Brown.
3. Eat to Nourish, Not Numb. Your body is screaming for fuel, not frosting. Lean into nutrient-rich foods that support neurotransmitter production—think leafy greens, nuts, eggs, and omega-3s.
4. Move Gently, but Move. Walk. Stretch. Flow. Don’t force a HIIT workout if your body says “nope.” Physical movement tells your brain you’re safe and helps flush out stress chemicals.
5. Gratitude & Reframing. This isn’t about Pollyanna-ing your pain away. It’s about giving your brain an alternate channel. Gratitude activates the prefrontal cortex, giving the limbic system (your emotional brain) a break. Try a nightly “3 good things” list.
6. Let the Emotions Out (But Not Take Over). Acknowledge the hard stuff. Feel it. Write it. Then gently move forward. Emotional constipation is just as real—and just as uncomfortable—as the physical kind.
7. The Core 4. It’s tempting to chase fancy fixes when everything feels off, but your foundation matters most. The Core 4—nutrition, movement, sleep, and stress management—are your non-negotiables. They stabilize your nervous system, refuel your brain, and keep your body from slipping further into burnout. Even small wins here (like hydrating well, moving your body gently, or getting 30 more minutes of sleep) can shift your chemistry and restore your capacity. These aren’t wellness hacks—they’re survival strategies.
8. Don’t Go It Alone. You can do hard things, but don’t have to do them alone. Whether it’s a trusted friend, a coach, or just someone who doesn’t respond with “just think positive,” connection is critical.
The Body Knows What It’s Doing. But It Needs a Partner!
Your body wasn’t designed to live in fight-or-flight forever. It’s trying to protect you, not punish you. If you feel heavy, drained, or stuck, that doesn’t mean you’re broken. It means your system needs rest, kindness, and recalibration.
I’m walking through this right now. And if you are, too, I want to say: it’s okay to slow down. You don’t need to earn your rest. You need to allow it. And if not today, find a way. Tomorrow is near.
How are you all hanging in there, health heroes? Let me know!
See you next week,
Dr Alice
A little more about Dr. Alice Burron and Strategic Action Health:
Dr. Burron is a co-founder of Strategic Action Health, dedicated to helping organizations help their employees make better health decisions. Come check us out here!
Catch us on Instagram: @the.health.navigator and @dr_burron
You can also connect on LinkedIn, if you want to be professional about it. 👓
Buy the book Health Shift here.
And if you’re not subscribed to Health Shift here on Substack, it’s time! This free newsletter is packed with valuable information and approaches to help you on your journey to better, faster healing.